Co-occurring disorder treatment: Gold Standard 2025
Understanding Co-Occurring Disorders and Your Treatment Options
Co-occurring disorder treatment addresses the simultaneous presence of a substance use disorder (SUD) and one or more mental health conditions. The most effective approach is integrated treatment, which means addressing both disorders at the same time.
When an SUD and a mental health condition exist together, they are called co-occurring disorders or a dual diagnosis. These conditions often influence each other, creating a difficult cycle where substance use can worsen mental health symptoms, and mental health challenges can lead to substance use as a coping mechanism.
This guide is your roadmap to understanding co-occurring disorders, why they happen, how they are diagnosed, and what effective treatment looks like. Our goal is to help you or your loved one find a path toward lasting recovery.
Basic co-occurring disorder treatment glossary:
What Are Co-Occurring Disorders (Dual Diagnosis)?
When we talk about co-occurring disorders, we’re referring to the simultaneous presence of a substance use disorder (SUD) and at least one other mental health condition. You might also hear this called “dual diagnosis” or “comorbidity.” The term “co-occurring disorders” is now preferred by organizations like SAMHSA (Substance Abuse and Mental Health Services Administration).
These conditions interact and often worsen each other’s symptoms. For example, alcohol use might temporarily ease anxiety but ultimately intensifies it, creating a self-perpetuating loop.
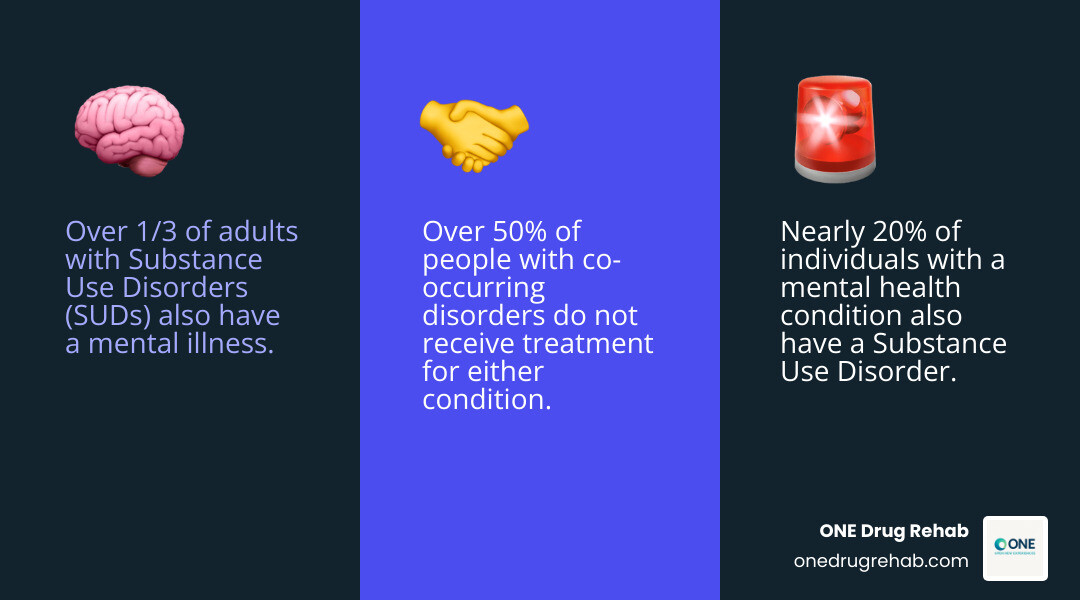
The prevalence of co-occurring disorders is high:
- Over a third of the 20.3 million adults with SUDs also have a mental illness.
- Nearly 20% of the 42.1 million people with a mental health condition also have a SUD.
- More than 50% of those with co-occurring disorders receive no treatment for either condition.
You can learn more from resources like the National Institute on Drug Abuse.
Commonly Co-Occurring Conditions
Some pairings of mental health conditions and SUDs are particularly common:
- Anxiety Disorders and SUDs: Individuals may use substances to self-medicate anxiety. About 18% of people with a SUD also have a co-occurring anxiety disorder.
- Depression and Alcohol Use Disorder: People may drink to cope with depression, but alcohol can worsen symptoms. A significant number of overdose deaths involve individuals with a depressive disorder.
- Bipolar Disorder and SUDs: The mood swings of bipolar disorder can lead to substance use to try and self-stabilize, which can exacerbate both the mood swings and the addiction.
- PTSD and SUDs: Trauma often drives individuals to use substances to numb the symptoms of Post-Traumatic Stress Disorder. People with PTSD are up to 4 times more likely to also have a substance use disorder.
- ADHD and SUDs: The impulsivity associated with Attention-Deficit/Hyperactivity Disorder can increase the risk of developing a SUD, with an estimated comorbid prevalence rate of 23%.
- Personality Disorders and SUDs: Conditions like Borderline Personality Disorder (BPD) have a very high rate of co-occurrence with SUDs, rising from 10-15% in the general population to 35-73% in patients treated for addiction.
These examples highlight why a comprehensive approach to co-occurring disorder treatment is essential.
The Complex Link: Why Mental Health and Substance Use Intersect
It’s often unclear which comes first, the mental health issue or the substance use. The relationship is complex, with several interconnected reasons why these conditions frequently appear together. You can explore more about this intricate relationship between Mental Health and Behavior.
Shared Risk Factors
Common underlying vulnerabilities can predispose a person to both conditions. These include:
- Genetics: A family history of mental health or substance use disorders can increase risk.
- Environmental Factors: Chronic stress and trauma are significant risk factors for both.
- Brain Chemistry: Both conditions can impact the brain’s reward system. Mental health disorders can make substances feel more rewarding, while long-term substance use can alter brain function, potentially triggering or worsening mental health issues.
The Self-Medication Hypothesis
A common theory is that individuals use substances to cope with or “self-medicate” untreated mental health symptoms. While this may offer temporary relief, it often makes the underlying problem worse in the long run, creating a vicious cycle.
The Bidirectional Relationship
The link is a two-way street:
- Mental Health Disorders Can Lead to SUDs: Self-medication and impaired judgment from a mental health condition can increase the risk of developing a SUD.
- SUDs Can Lead to Mental Health Disorders: Long-term substance use can trigger or worsen mental health conditions. Withdrawal can also mimic or intensify symptoms of mental illness.
Understanding this interplay is crucial for effective co-occurring disorder treatment.
Common Signs and Symptoms
Spotting co-occurring disorders can be tricky due to overlapping symptoms. Key signs include sudden behavioral changes, social withdrawal, neglect of responsibilities, and relationship or financial problems. Physical signs might include bloodshot eyes or changes in weight. A key indicator is needing to use substances just to feel “normal.”
Mental health symptoms may also worsen, including extreme mood swings, confused thinking, and an inability to function in daily life. Thoughts of suicide or self-harm are critical warning signs that require immediate professional help.
Why Diagnosis Can Be Challenging
A professional diagnosis is crucial but can be difficult for several reasons:
- Symptom Overlap: Symptoms of substance intoxication or withdrawal can mimic those of mental health conditions.
- Substance-Induced Symptoms: It’s hard to tell if a symptom is from an underlying disorder or caused by substance use. A period of abstinence is often needed for an accurate diagnosis.
- Patient Factors: Shame or fear may prevent individuals from being fully open about their substance use.
- Lack of Integrated Training: Historically, mental health and addiction specialists worked in silos, leading to fragmented care.
A thorough, professional assessment is the essential first step toward an effective co-occurring disorder treatment plan.
The Gold Standard: Integrated Co-Occurring Disorder Treatment

Historically, mental health and substance use were treated as separate issues. This approach proved ineffective for co-occurring disorder treatment.
Today, “integrated treatment” is the gold standard. This means both the mental health condition and the SUD are treated at the same time, by the same team, in the same program. It’s a holistic approach that views you as a whole person.
SAMHSA strongly recommends integrated care because it leads to better outcomes, including reduced substance use, improved mental health symptoms, a higher chance of lasting recovery, and a better quality of life. You can review guidelines on integrated treatment to understand its importance.
The Diagnostic and Treatment Process
Your journey begins with a comprehensive assessment, including your medical history, a mental health evaluation, and a review of substance use patterns. This helps professionals understand how your conditions are connected.
From this assessment, a personalized treatment plan is created to fit your specific needs and goals. Co-occurring disorder treatment is offered in various settings, and ONEDrugRehab.com can help you find facilities offering different levels of care:
- Detoxification: Medically supervised withdrawal management for physical dependence.
- Residential Treatment: Living at a treatment center for structured, 24/7 support, ideal for serious co-occurring disorders.
- Outpatient Programs: Living at home while attending regular therapy. This includes intensive options like Partial Hospitalization Programs (PHPs) and Intensive Outpatient Programs (IOPs), which are great for those with stable home environments or as a step-down from residential care.
The goal is a “no wrong door” approach, ensuring that anyone seeking help is screened for both conditions and guided toward integrated care.
Key Therapies in Co-Occurring Disorder Treatment
Integrated treatment uses a mix of proven therapies to teach coping skills and address underlying issues:
- Cognitive Behavioral Therapy (CBT): Helps identify and change negative thought patterns and behaviors.
- Dialectical Behavior Therapy (DBT): Teaches skills in mindfulness, emotion regulation, and distress tolerance, which is especially helpful for intense emotions.
- Motivational Interviewing (MI): A collaborative approach to help you find your internal motivation to change.
- Trauma-Informed Care: An approach that recognizes and responds to the impact of trauma, ensuring a safe and supportive treatment environment.
- Family Therapy: Involves loved ones to improve communication, set healthy boundaries, and heal relationships.
- Support Groups: Peer groups like AA, NA, and Dual Diagnosis Anonymous (DDA) offer valuable community and shared experience.
The Role of Medication in Co-Occurring Disorder Treatment
Medication can be a vital component of co-occurring disorder treatment, used alongside therapy. A medical professional will determine the appropriate medications and dosages.
- For Substance Use Disorders (SUDs): Medications like buprenorphine and naltrexone for Opioid Use Disorder, or naltrexone and acamprosate for Alcohol Use Disorder, can reduce cravings and support sobriety.
- For Mental Health Conditions: Antidepressants can help with depression and anxiety. Mood Stabilizers are used for conditions like bipolar disorder. For ADHD, Stimulants can sometimes reduce impulsivity and substance use risk when carefully monitored.
Combining medication management with therapy is a hallmark of high-quality co-occurring disorder treatment.
Finding Help and Embracing a Hopeful Future
Starting on co-occurring disorder treatment is a courageous step toward a hopeful future. Effective, integrated treatment dramatically improves overall quality of life.
Benefits include:
- A greater sense of well-being and happiness.
- Stable housing and better relationships.
- The ability to return to work or school.
- Fewer hospitalizations and legal issues.
- Improved physical health.
Despite these benefits, barriers like stigma and cost can make seeking help feel daunting. However, laws like the ACA and MHPAEA mandate that most insurance plans cover mental health and substance use treatment, making care more accessible.
How to Find the Right Support
Finding the right co-occurring disorder treatment program is critical. Not all facilities offer the comprehensive care needed.
- Prioritize Integrated Treatment: Look for facilities that explicitly offer dual diagnosis programs. Only about half of treatment centers do, so it’s important to ask.
- Ask Key Questions: When contacting providers, ask if they offer integrated treatment, how they assess for both conditions, what therapies they use, and if they provide medication management.
- Verify Credentials: Ensure staff are licensed and experienced in treating co-occurring disorders.
- Consider Your Needs: Think about location, specialized programs, and insurance coverage.
ONEDrugRehab.com is a third-party, non-affiliated resource to help you research treatment options and make an informed choice.
Resources for Families and Young Adults
Family involvement is vital for long-term recovery. Support systems provide encouragement, accountability, and a safe space for everyone involved.
- SAMHSA Resources for Families: SAMHSA’s website offers guidance for families on finding support and helping loved ones.
- NIDA Resources for Parents and Educators: NIDA provides resources for parents and educators to understand addiction and start conversations with young people.
- Peer and Family Support Groups: Groups like Al-Anon, Nar-Anon, and NAMI offer safe spaces for family members to share experiences and reduce feelings of isolation.
You don’t have to steer this alone. Seeking support is a sign of strength.
Frequently Asked Questions about Co-Occurring Disorder Treatment
It’s normal to have questions when considering co-occurring disorder treatment. Here are answers to some common questions.
Can you treat a substance use disorder without addressing the mental health condition?
Not effectively. When a mental health condition and a SUD are present, they are deeply connected. Trying to treat one without the other often leads to a high risk of relapse, as the untreated symptoms of one condition can fuel the other. This is why integrated co-occurring disorder treatment, which addresses both simultaneously, is the gold standard for care. It tackles the root issues, not just the surface symptoms, leading to more stable, long-lasting recovery.
How long does co-occurring disorder treatment take?
There is no single timeline for co-occurring disorder treatment. The duration depends on the severity of the disorders, individual progress, and the level of care required. Treatment is a continuum, often moving from more intensive care (like 30-90 day residential programs) to less intensive support (like outpatient therapy). Recovery is a long-term process, and many people find that ongoing therapy and support groups are valuable for maintaining their well-being for years.
Is relapse a sign of treatment failure?
Absolutely not. Relapse is a common part of the recovery process for chronic conditions like SUDs and mental illness. It is not a sign of failure but rather an indication that the treatment plan may need adjustment. A relapse can be a powerful learning opportunity to better understand triggers, strengthen coping skills, and reinforce the commitment to recovery. It highlights the importance of ongoing support to get back on track.
Conclusion
We hope this guide has clarified co-occurring disorder treatment and provided a hopeful roadmap forward. We’ve seen how common and intertwined these conditions are, but the most important takeaway is this: recovery is absolutely possible through the right approach.
The key is integrated treatment. Addressing both mental health and substance use disorders simultaneously creates a powerful healing process that leads to lasting, positive change.
If you or someone you care about is struggling, please know you are not alone. Taking the first step is a courageous decision toward a healthier, more fulfilling life.
ONEDrugRehab.com is here to be your trusted companion. As a third-party, non-affiliated resource, we are dedicated to providing clear information to help you research treatment options and make an informed decision.
Your path to recovery is unique, but a future filled with hope and healing is well within reach.
Find a treatment center that specializes in co-occurring disorders




